If you have tried other treatments for UC (ulcerative colitis) and they have not been effective, ulcerative colitis surgery might be the recommended solution. You may also opt for surgery if you want to eliminate your risk of colorectal cancer and avoid further complications. At the Colorectal Division of North Carolina Surgery at UNC REX in Raleigh, ulcerative colitis surgery is performed by our highly experienced colorectal surgeons.
What is Ulcerative Colitis?
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that causes inflammation and ulcers in the lining of the colon and rectum. This condition can lead to severe digestive issues and significantly impact daily life.
Common symptoms include:
- Persistent diarrhea with blood or pus
- Abdominal pain and cramping
- Fatigue
- Urgency to have a bowel movement
- Unintended weight loss
- Fever
How Do I Know If Surgery Is Right For Me?
Deciding if UC surgery is the correct course of action depends on several factors, including the severity of your symptoms, how well your body responds to medications, and the presence of complications such as severe inflammation, colorectal cancer, or bowel perforation. Surgery is typically considered when non-invasive treatments no longer control symptoms effectively or when complications pose significant health risks.
Surgical Options for Ulcerative Colitis
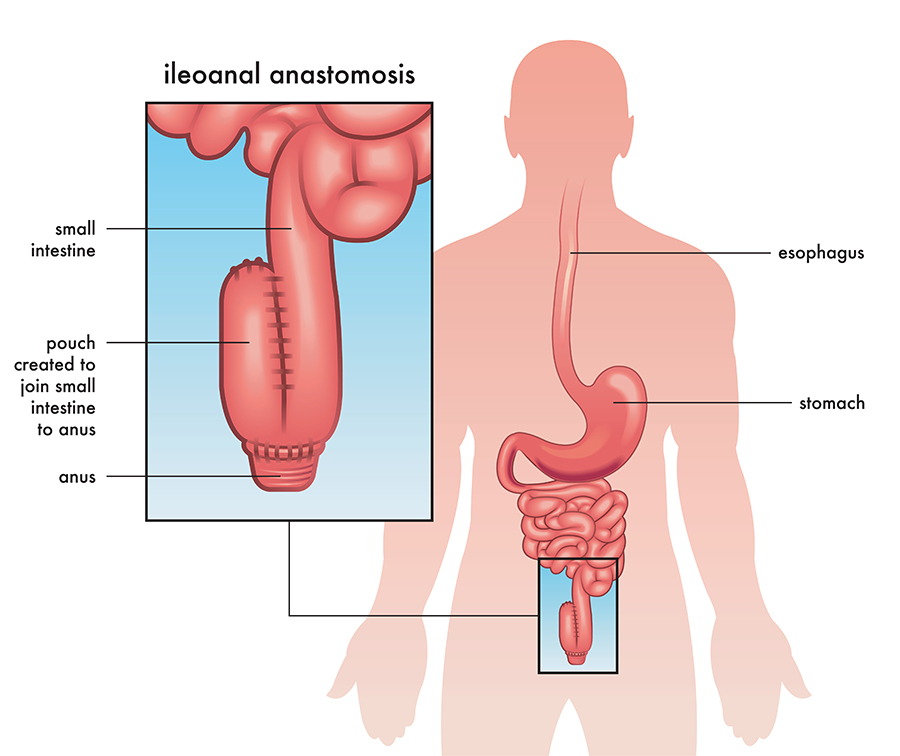
Surgery for ulcerative colitis involves removing the diseased tissue in your digestive tract. The two main surgical procedures for UC are:
Proctocolectomy With Ileal J-Pouch Creation
This procedure is the most commonly recommended elective surgery to cure UC. Doctors begin with a proctocolectomy to remove the colon and rectum. They then replace those organs with a J-pouch, which is created from your small bowel and made to function similarly to a rectum for bowel elimination.
Your surgeon may recommend a one-, two- or three-stage procedure, each allowing your body a different amount of time to heal between removing your diseased organs and replacing them with the J-pouch. Your surgeon will discuss which approach is best for you based on your specific health factors.
Proctocolectomy or Colectomy with End Ileostomy
In this procedure, your surgeon removes the diseased colon and/or rectum. Afterward, they will create an ileostomy, which connects to an ostomy pouch to collect waste outside your body. Your specialist might recommend this procedure if you have other severe conditions that can put you at high risk for further complications.
Living with an ostomy bag can take some getting used to. The team at UNC REX will provide the support and resources you need to get back to living your best life.
Benefits of Ulcerative Colitis Surgery
- Relief from severe symptoms like pain and persistent diarrhea
- Elimination of diseased tissue to prevent future complications
- Significant improvement in quality of life and daily functioning
- Reduction or elimination of long-term medication use
- Lowered risk of colorectal cancer
Schedule an Appointment
If you are experiencing persistent symptoms and are considering ulcerative colitis surgery in Raleigh as a treatment option, our dedicated team is ready to assist you. Get in touch with the Colorectal Division of North Carolina Surgery at UNC REX to set up your first appointment.
Frequently Asked Questions
Will I be able to live a normal life after UC surgery?
Yes, most people can live a normal and active life after UC surgery, though adjustments may be needed depending on the type of procedure performed. With proper recovery, dietary management, and medical support, patients often experience significant symptom relief and improved quality of life.
Will I need to take any medication after UC surgery?
While surgery may eliminate the need for certain UC medications, some patients may still require medicine to manage inflammation, prevent infections, or address complications like pouchitis. Your doctor will determine the best post-surgical treatment plan for you.